Black technology is coming - cool BioBots will set off a wave of 3D printing of living cells
Release date: 2015-05-12
BioBots is an American biotechnology startup with a focus on computer science and chemistry. The company's first product is a 3D printer that prints biomaterials and was recently unveiled at the TechCrunch Disrupt conference in New York. According to co-founder Danny Cabrera, the printer combines hardware, software and wetware (the brain's nervous system, corresponding to computer hardware and software), and the wet parts part of them reflect their Core innovation technology.
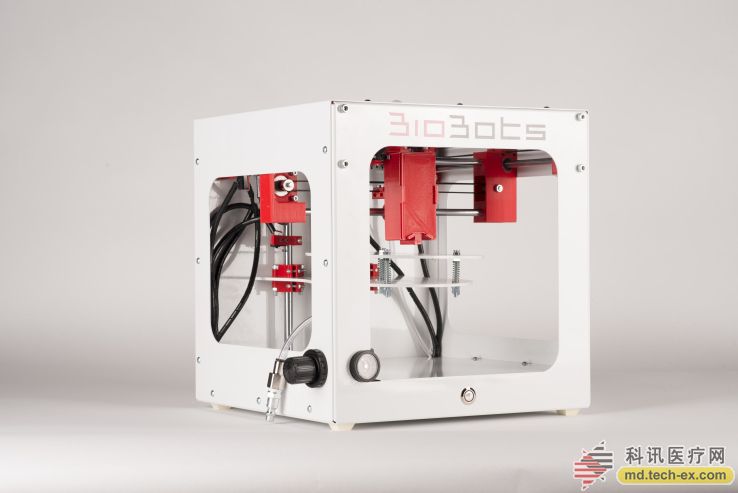
Biomanufacturing is the process of artificially making a living biological tissue structure. This is not an emerging field, and people have been studying it for decades. But Cabrera and his co-founders are convinced that they have discovered a new business opportunity to replace the traditionally expensive (over $100,000), bulky and complex equipment with new equipment. According to reports, they are inspired by small and low-cost desktop 3D printers.
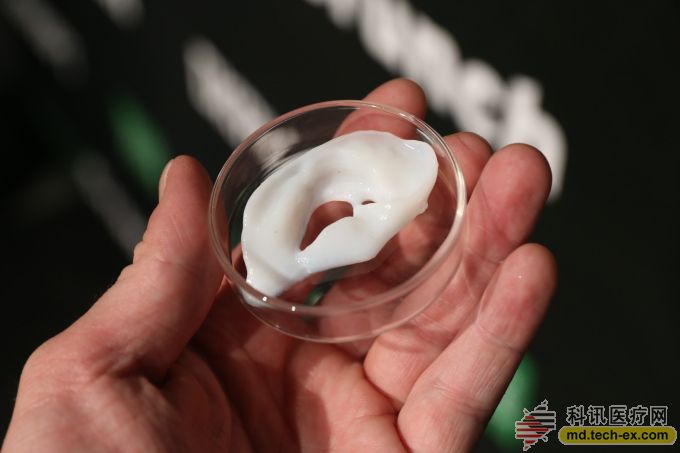
Ordinary 3D printers use plastic for printing, while BioBots' 3D printers use special inks. This ink consists of biological materials and living cells that can be used to print 3D living biological tissues and miniature human organs. Currently, the products they print can be used for screening before scientific research and clinical stages, such as replacing animals for drug testing. Although the field of biomanufacturing is gradually moving toward the manufacture of alternative human organs, BioBots is still unable to use human cells to print out replaceable organs. According to Cabrera, in the short term, the potential use of the company's technology will be to help develop specific disease treatments.
He said: "We really just regard this device as a pharmaceutical company's product, only for clinical drug testing. You can use the human cell to print out the living biological tissue model with the help of our equipment, and these models are more than Traditional 2D organizations are more complex and sophisticated. These printed tissue models summarize the functions of the human body, and you can use them to develop compounds for clinical practice, so that you can find false positives before entering the clinical trial phase. Case."
“We think this technology is a way to develop a personalized treatment plan. After the patient comes to the clinic, doctors can directly extract their cells and print 3D tissue, micro-tissue, and then use these personalized products to test different treatments for patients. Program, drug efficacy. Similarly, doctors can also develop personalized treatments for patients with specific conditions."
“In the traditional method, we grouped some diseases into one category and gave them a name. But these diseases are different in each person's performance. And the drug development process is not keeping up with the times – we are always In an expensive clinical trial, we developed a drug that can be applied to thousands of patients, but we can't develop personalized drugs. But today, technology makes personalized drugs a reality, we can develop a drug for a patient alone. He added.
BioBots was originally an entrepreneurial project that originated in a university residence. In July last year, when the two co-founders received degrees in computer science and biology from the University of Pennsylvania, they became interested in genetic engineering and tissue engineering.
Cabrera said: "Our idea is that we can use the same way as traditional 3D printers to create a smaller, cheaper biotech device. At the time, the equipment in the traditional bio-manufacturing sector was huge. It looks like an old computer host that can occupy the entire room. And those devices usually cost $500,000 and are very difficult to operate. You need to find a professional technician to get the job done."
BioBots won $5,000 in the early days of the University of Pennsylvania and developed their first prototype. Since then, they have successfully sold a device to a Ph.D. student and passed the screening of the Dreamit Health Accelerator Program in Pennsylvania. They joined the project last fall and received $50,000 in funding. Currently, the company's first generation of biomaterial printing equipment has been shipped. They work closely with researchers to continually debug their first generation products. It is reported that if researchers are willing to help BioBots in research and development, they will buy this 3D printing device for $5,000.
Their business model is to sell different types of ink to researchers, and different inks can print different biomaterials. They launched a beta version of the Cartilage Tissue Ink Kit for $700.
BioBots' printers use blue visible light and a complex photoinitiator with specific inks to process biological tissue, rather than using UV and pressure to finish printing like other devices. Cabrera said that their method is more efficient, because the use of pressure and ultraviolet light to print living tissue can damage living cells, while blue visible light does not adversely affect cells.
To use this device to create biological tissue (such as a piece of bone, cartilage, or liver), users need to assemble the company's photoinitiator powder with the living cells they want to print. At the same time, they also need to add binding factors to ensure that the cells bind together.
Cabrera explained: "Our ink consists of three powders. Users need to add the binding factor and the living cells they want to use. Wait for 5-10 minutes after mixing, then add these substances to the printing device. We need to use CAD design software such as AutoCAD and Solidworks to complete the structural design work. Our software can convert the design files into instructions that the printer can recognize."
BioBots' 3D printers have an internal press that uses hydraulic pressure to squeeze the material out of the nozzle. Once the biomaterial is printed, the device uses blue visible light to complete the structural hardening. The time of printing varies depending on the content of the print, depending on the type of tissue you are trying to make.
“So far, our customers have printed bones, lungs, liver, heart, brain, skin and cartilage,†Cabrera said.
The Techcrunch website interviewed Cabrera about BioBots' 3D printer.
Q: What is your distribution strategy? How do you plan to sell your equipment to hospitals and doctors? Can medical insurance reimburse printing costs?
A: At this stage, our products are more of a research tool. We are working hard to market this device to pharmaceutical companies and negotiate with their R&D department. So at the moment we have no contact with the doctor, just dealing with the researchers. We have many existing channels that can be sold to pharmaceutical companies. At the same time, we are also looking for partners, hoping to reach a cooperation with pharmaceutical companies.
Q: You have a lot of partners. Do you give you feedback and data on the equipment? Are they using your device? What organization did they print?
A: The customers I show are early adopters who bought the printing device before we launched the ink kit. They will tell us everything they do, like how to use the device. This gives us a lot of information and data on tissue engineering. With their help, we discovered that a cartilage tissue ink kit should be introduced. R&D centers in the bio-manufacturing sector spend tens of millions of dollars on research, and our equipment accelerates their R&D.
Q: How do you define success? Do you think equipment sales are successful? Is the current sales situation the same as your vision?
A: Our equipment is a mechanical system itself, so it can be measured in a very simple way – resolution and accuracy. Of course, this is closely related to the researchers who use the equipment and their work. For example, for pharmaceutical companies, they need to print microscopic tumors and test them to see if the drugs are effective. We hope that the printed tissue will have the basic functions of the human body and show the activities of the human body. If we can do this, our equipment will be successful. If we can't do this, then we have to start all over again. That's what digital manufacturing technology means – reducing turnaround time and helping you quickly change your design.
Q: Can you use your equipment in the field of organ replacement? In many basic research in life sciences, you can develop a skin graft specimen and test the drug on it. How do you see this replacement?
A: First of all, the tissue we print will not replace any human tissue. In the traditional mode, we can only create 2D organizational samples, and now our equipment gives you the ability to create 3D organizations. This is significant in terms of physiology. The cells in 3D are completely different from the 2D state, so pharmaceutical companies are very excited about our technology and have said that this is what they have been looking for. Europe has banned the use of animals for cosmetic testing, so the tissue printed by our equipment has its place to use, and it can replace animals to complete experiments. I believe that in the future, our printers will be able to print tissue organs that can completely replace the clinical development of drugs.
Ideally, we all want to test individualized drugs specifically developed for individuals. But the problem is that no one wants to be a mouse. However, our equipment is capable of printing 3D tissue through the patient's cells for drug development. In this way, the researcher does not need to conduct an experiment on the patient himself, but can test the structure of the drug.
Q: There are other companies in the market that manufacture 3D printers in the medical field. Can you introduce the technology that you use without killing cells? How did you develop this technology without a lot of financial support? How reliable is this technology? What do other people do to imitate your technology?
A: I am a student at the University of Pennsylvania. After graduation, I met a friend (the other founder of the company, Ricardo), who was developing prototype equipment for our current products. After graduation, we stumbled upon a chemical that people used for a variety of other different uses. We were looking for a technique that did not damage cells and then found a compound. It combines with visible light to achieve the desired effect. We tested it and it worked very well. Previously, no one had applied for a patent for visible light technology in the field of 3D printed living tissue. Therefore, we feel that this is an opportunity. Moreover, this technique is also biologically plausible. We filed a patent application earlier this year. We believe this technology is reliable. And it is not only reliable, but also the best way to make living tissue.
Source: Singularity Network
Freeze Dried Food,Freeze Drying Sea Shrimp,Food Hyaluronic Acid Powder,Freeze Dried Carrot Powder
Ningbo Nutrition Food Technology Co.,ltd. , https://www.collagenworkshop.com